One aspect of the Search for an Attenuated Natural strain via Epidemiology (SANE) that I have not discussed in depth is the use of an attenuated SARS-CoV-2 strain as tool to accelerate the development of a vaccine for COVID-19.
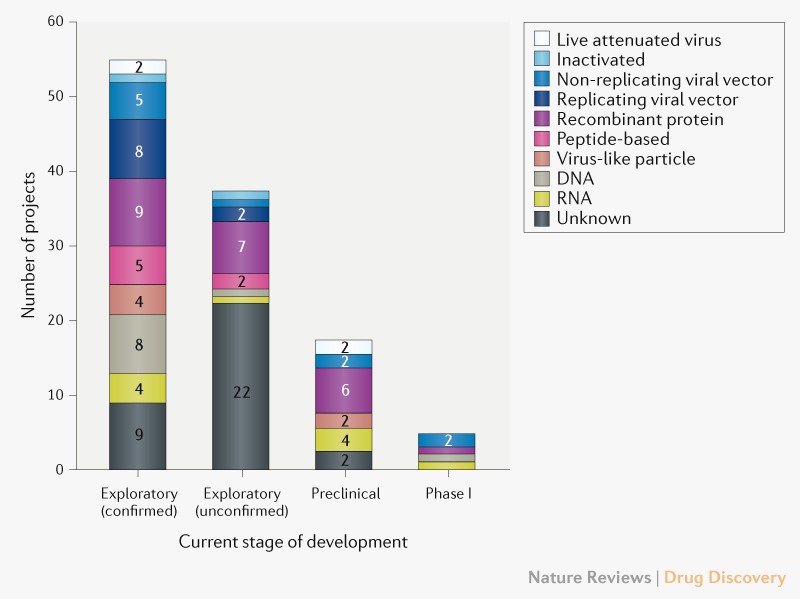
There are now nearly 100 different SARS-CoV-2 vaccines in various stages of development, although only 5 are in Phase 1. Nature Review Drug Discoveries has published an excellent review on all the different vaccine approaches. There is an enormous scientific and financial effort going into all these programs, but when will we have a vaccine?
Vaccine Development Bottlenecks
Vaccine development has a number of significant bottlenecks. Assuming you have a vaccine candidate that appears safe in preclinical and early stage human testing (Phase I & II), the major hurdle you must overcome is showing your vaccine actually works in the real world. This often requires large scale Phase III human field trials where you vaccinate 10,000s to 100,000s of people and then monitor them over time to see if they are protected from the disease. For example, the Francis Field Trial of the Salk Polio Vaccine in 1955 involved vaccinating 440,000 children in the USA, along with 210,000 children getting placebo injections, and 1.2 million additional children used as controls. The 1961 Sabin Oral Polio Vaccine Phase III trial involved vaccinating 10 million childrenin the Soviet Union. These were truly heroic trials to show these vaccines worked.
An alternative to running huge Phase III field trials is the challenge trial. With this approach you test if your vaccine works by exposing a relatively small numbers of volunteers to the disease and seeing if the vaccine protects them from getting infected. By using deliberate exposure you can limit the number of people you need to put at risk to determine if a vaccine works.
Ethics of Vaccine Development
Developing a new vaccine raises many ethical dilemmas. Do you expose your volunteers to the disease to see if it works (challenge), or do you instead expose large numbers of people (field trial) to a vaccine that may not work? >
If your vaccine is for a disease for which there are good drug treatments (e.g. malaria), or if the disease is mild (e.g. the common cold), then the challenge approach can be an ethical way to show a new vaccine works. If the disease is dangerous (e.g. HIV), then you must use a field trial approach as it is not ethical to deliberately expose people to a deadly disease.
Beyond the ethics of these different approaches, there are practical concerns too. Not only are large field trials much more expensive, they takes much longer than a challenge trial as the logistics of vaccinating and monitoring hundreds of thousands of volunteers is not trivial. In times of a pandemic like we have with COVID-19, every day of delay results in the deaths of many thousands of people.
Ethical Dilemma of a SARS-CoV-2 Vaccine
COVID-19 raises some unique ethical issues. We want an effective vaccine as quickly as possible, but COVID-19 is a deadly disease for which we currently have no effective treatments. Large scale Phase III field trials will take many months to run even once we have vaccine candidates ready to test (we are nowhere near being ready to run such a field trial). Some people have suggested that we expose young and healthy volunteers to SARS-CoV-2 after vaccination to speed up the vaccine development process (i.e. run a challenge trial). More than 1500 people have signed up to participate in such a trial.
The important question we have to consider is if it is ethical to deliberately expose even the young and healthy to the dangerous SARS-CoV-2 virus when we know it could seriously injure or kill them. It might be justified if there were no alternatives, but if we had an attenuated/mild strain of SARS-CoV-2, nobody would even think of using a dangerous strain in a challenge study as it would be completely unethical. It is only the lack of an attenuated strain of SARS-CoV-2 that leads people to even contemplate using a pathogenic strain in a challenge trial.
The Ethics of not Looking for an Attenuated SARS-CoV-2 Strain
If we know it would be unethical to use a dangerous pathogenic strain of SARS-CoV-2 in a challenge trial if we had an attenuated strain, and if we know how to look for an attenuated strain, how can it be ethical to not search for such a strain? How is it ethical to consider exposing people to a dangerous virus just because we can’t be bothered to look for a safer strain?
The only conclusion we can draw is the search for a natural attenuated SARS-CoV-2 strain is an ethical imperative even if the chance of success is low. We can not ask our COVID-19 vaccine volunteers to put their lives on the line for us just because we thought it would be too difficult to look for a safer strain. Convenience is never a justification to act unethically.
